Abstract
Background:
Follicular lymphoma (FL) is the most common indolent non-Hodgkin lymphoma. The initial management varies from watchful waiting to a combination of chemoimmunotherapy (CT) and radiation therapy (RT). Goldstein et al. recently reported (Blood, pre-published online, July 24 2018) that FL patients with no insurance or Medicaid had worse OS. We examined whether the survival discrepancy was caused by access to initial treatment using the National Cancer Database (NCDB).
Methods:
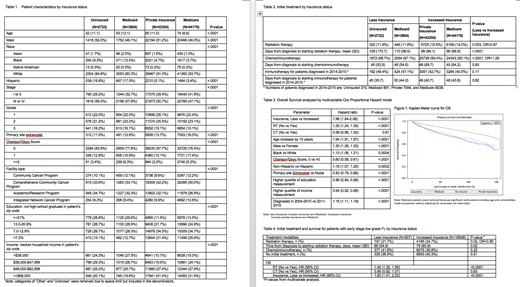
FL cases diagnosed from year 2004-2015 in NCDB were included. Demographic characteristics were compared using Chi-square test for categorical variables and ANOVA for continuous variables. Use of CT and RT was analyzed in multivariate logistic regression including the following variables: age, gender, race, Hispanic ethnicity, stage, grade, primary site extranodal, facility type, urban/rural location, distance to facility, year period of diagnosis (2004-2010 vs 2011-2015), education, income and insurance status. Overall survival (OS) was analyzed using Cox proportional hazard model including the same covariates with addition of CT and RT.
After Jan 2013, rituximab was captured as immunotherapy. To assess the use of rituximab, we compared immunotherapy in years 2014 and 2015 to avoid possible data entry error in 2013.
The treatment modalities and OS were similar for uninsured and Medicaid patients, and for Private and Medicare patients after adjusting for covariates. We combined "uninsured" and "Medicaid" into "Less" insurance and "Private" and "Medicare" into "Increased" insurance.
Results:
A total of 94057 FL cases were included in the analysis with the following insurance status: Uninsured 2723 (2.9%), Medicaid 3804 (4.0%), Private insurance 43354 (46.1%), and Medicare 44176 (47.0%).
Patients with no insurance or Medicaid were more likely to present at an advanced stage (Table 1).
In the multivariate model, less insurance was associated with less initial use of radiation therapy (OR=0.87, p=0.003) and more use of CT (OR=1.28 p<0.0001). For patients diagnosed in years 2014 and 2015, initial use of immunotherapy (most likely rituximab) and the waiting time before starting immunotherapy did not differ by insurance status.
Both less insurance and not-receiving radiation therapy were associated with worse OS after adjusting for covariates (HR=1.96 and 1.30, respectively, p<0.0001 for both, Table 3, Figure 1). Chemoimmunotherapy was not associated with OS. Lower education and income were both associated with worse OS after adjusting for insurance (Table 3).
RT is recommended as frontline treatment for suitable patients with early stage (stage I/II) low grade (grade 1/2) FL. We analyzed the use of RT and survival outcome in this patient group. The results were similar to results for the entire patient set. Patients with less insurance received RT less often (21.7% vs 24.7%, p=0.02), and when they did receive radiation therapy, the waiting time before starting treatment was longer (89 days vs 79 days, respectively, p=0.02). Both less insurance and not-receiving RT were associated with worse OS (p<0.0001 for both, Table 4).
Conclusion:
Follicular lymphoma patients with no insurance or Medicaid had worse OS. Less insurance was associated with decreased access to initial radiation therapy but not chemoimmunotherapy. However the survival discrepancy cannot be solely explained by access to radiation therapy given the magnitude of difference. Moreover, insurance remains a significant predictor of survival after adjusting for initial treatment. The key drivers of the survival discrepancy by insurance status in FL patients need to be further defined.
Feldman:Portola: Research Funding; KITE: Speakers Bureau; Celgene: Speakers Bureau; Pharmacyclics: Speakers Bureau; Janssen: Speakers Bureau; Seattle Genetics: Research Funding, Speakers Bureau; Johnson and Johnson: Speakers Bureau. Chang:Incyte: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal